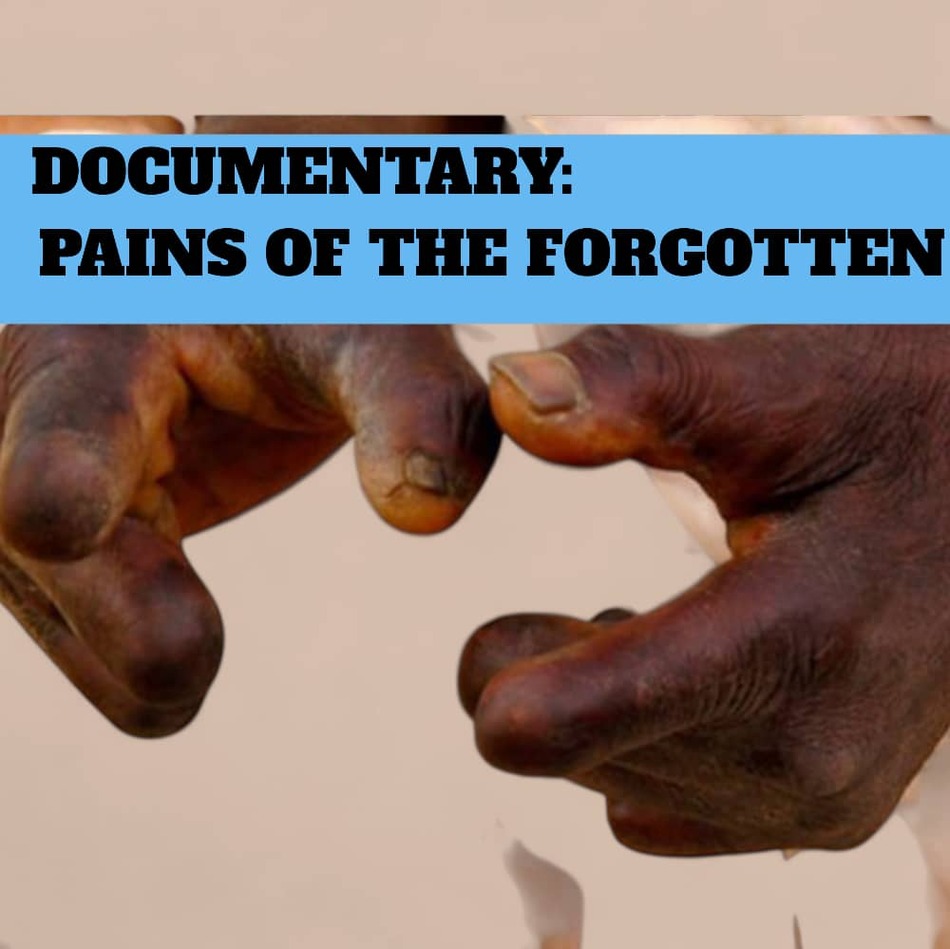
Between January 2019 and October 2025, the Upper East Region of Ghana quietly recorded 188 cases of leprosy, a disease as old as civilization, yet as misunderstood and feared as ever. Apexnewsgh reports These numbers, dry on paper, conceal stories of courage and struggle, of families fractured and communities forever changed. At the center of this unfolding story is Eric Dakura, the Disease Control Officer at the Upper East Health Directorate, whose daily work illuminates the dark corners where leprosy still hides. Eric’s insight and passion were brought to light in the documentary “Pains of the Forgotten: Leprosy, Stigma, and Resilience,” produced by Ngamegbulam Chidozie Stephen of ApexNewsGH. With a clinical calm that betrays deep empathy, Eric decoded the disease for viewers: “Leprosy is a disease of the skin and the nerves. If you don’t get the treatment early, it will affect your nerves and finally lead to the wasting of your feet or your fingers, and that can lead to disability.” Unlike most diseases, leprosy’s touch is silent. Its symptoms can take years—sometimes three, five, even twenty- to appear after infection. “It’s not like any other disease that when you get infected within a week or two weeks, you get the signs and symptoms,” Eric explains. “It can be in you for over three years, up to twenty or even more years until it begins to manifest.” The first warning is often a pale, painless patch on the skin. Because these patches neither itch nor hurt, they are easily dismissed—until the disease has already begun its devastating work. “Leprosy doesn’t cause pain,” Eric says. “That is why you can see somebody with their fingers being chopped off, but there is no pain… if you even put them into fire, they will never feel anything because the nerves are all destroyed.” The destruction of nerve endings is what makes leprosy so dangerous and so easy to miss. Eric recalls a haunting case from his rounds: “A girl found a three-inch nail in her foot last year. She didn’t even know it was there because all the nerves were affected.” By the time many are diagnosed, the disease has already stolen their ability to feel, to move, or even to recognize when they are hurt. Early detection remains the greatest challenge. “We always get to know leprosy at a later stage, when the hands and the feet are gone. We don’t want to be recording cases at that stage because it means that our surveillance system is not the best.” The region now grades leprosy cases by disability: some show no deformities, some suffer numbness, while others arrive with missing fingers, feet, or affected eyes. Leprosy is endemic in all districts, but certain areas—like Bongo—have become persistent hotspots. There is progress, though: the annual number of new cases has dropped, from 32 in 2020 to just 16 currently on treatment. Yet Eric cautions that declining numbers are not always comforting. “If we record a lot of cases, it’s also good—meaning we are fishing out the hidden cases and treating them. But if we feel the numbers are declining, that could also be dangerous. We must always be on the watch.” Leprosy respects no boundaries. It is not hereditary, nor confined to the poor or the old. “Seventy percent of cases are male, but the youngest can be just two years old,” Eric shares. “There is no age that is exempted. Everybody, males, females, we are all at risk of getting it.” Yet there is hope, because leprosy is curable. “Leprosy is curable. That has always been the slogan. Just come, we’ll treat you and you’ll be fine,” Eric says, his tone unwavering. The medication, though costly for the government, is provided free of charge. “Wherever you are, the medicine can come to you, even your home.” But for all the medical progress, the greatest struggle is not clinical, but social. The shadow of stigma still looms large. “If you are affected, and unfortunately you lose your legs, there’s no way the person will be able to make life meaningful for himself. Even my own children, they dissented me. People that I used to eat with, they can’t eat with me,” Eric recounts, echoing his patients’ pain. He urges empathy and shared responsibility: “The fact that it hasn’t manifested in you doesn’t mean you don’t have it. So we just have to believe each other as people. When somebody has a problem, that is also your problem.” Often labeled a “disease of the poor,” leprosy’s grip is strengthened by poverty and neglect. “Almost all the people who are largely affected are people who come from poor living conditions. Eighty to ninety percent of the cases are in Africa. Because Africa is highly impoverished,” Eric explains. Still, hope guides his work. Through outreach, education, and persistent surveillance, the region edges closer to a day when leprosy is history. “If we get to a point where in a population of about 10,000, only one person is likely to have it, that is the aim,” Eric says. “So, in years to come, a generation will come that will not suffer from this kind of disease.” Until then, the story of leprosy in Ghana’s Upper East is one of vigilance, hope, and the unyielding human spirit, a story that, thanks to people like Eric Dakura, is no longer shrouded in shadows but moving steadily toward the light. WATCH THE VIDEO DOCUMENTARY: Source: Apexnewsgh.com/ Ngamegbulam Chidozie Stephen
Breaking the Chains of Stigma: Tahiru Suleman’s Fight for Inclusion in Bongo
Where the red earth stretches beneath acacia trees and the air hums with the rhythm of rural life, one man’s voice rises above the silence that too often surrounds the lives of leprosy survivors. Apexnewsgh reports Tahiru Suleman, the Assistant Assembly Member for the Awukabisi Electoral Area, is on a mission to transform not just policies, but hearts and minds. Tahiru’s journey began with a simple but painful observation: “In our community and electoral area, we have a lot of people suffering from leprosy. Just within my electoral area, I can pinpoint about four or five people who are infected.” Yet the challenges facing these individuals go far beyond their diagnosis. Their true struggle is against an invisible enemy: stigma. This hard reality was laid bare in the documentary “Pains of the Forgotten: Leprosy, Stigma, and Resilience,” produced by Ngamegbulam Chidozie Stephen of ApexNewsGH. Tahiru, speaking with a blend of compassion and urgency, described what he saw: “These people go through a lot. When they are seen in public, people run away from them. Some even think that if the saliva of someone with leprosy touches them, they will be infected.” For those living with leprosy, every day is a test of endurance. Beyond the pain of their disease is the pain of rejection. Tahiru detailed the myths that persist, deeply rooted in local lore: “Some people think leprosy is a curse from certain families, but that is not true. Leprosy can attack anybody.” To make his point, he shared the story of a close colleague who, despite years of good health, unexpectedly contracted leprosy. “If someone had told him in the past that he would have this disease, he wouldn’t have believed it.” The stigma is isolating. Many affected individuals lose their livelihoods, shunned not just by neighbors but sometimes even by their own families. “Because of the disease, some of them cannot do any active work. Even within their families, people don’t want to associate with them. For some, even getting food to eat is a big problem,” Tahiru explained, his voice heavy with empathy. Moved by these injustices, Tahiru has become an outspoken advocate for change. He passionately calls upon health authorities, NGOs, and the general public to intensify education about leprosy. “What they need is love, not rejection. We must all help fight the stigma.” But Tahiru’s campaign does not end with leprosy. He recognizes that those living with Neglected Tropical Diseases (NTDs) across Bongo face similar challenges. “I think it is our responsibility as Assembly Members to educate the community members about the ongoing stigmatization and discrimination against people living with NTDs in our communities,” he said. Public education, he believes, is the most effective antidote to fear and ignorance. “There is a need for people to know the dangers of discriminating against these people.” Yet, progress is not easy. Tahiru describes the frustration of working alone: “Our challenge has to do with community members not listening to us individually in this direction.” His answer is to build partnerships with health workers, who bring not only expertise but also credibility to community education efforts. “There is a need for health workers to make themselves available for such exercises in the community.” For Tahiru, real change will come only when local leaders, health professionals, and ordinary citizens unite in purpose and compassion. He envisions a future where those affected by NTDs can walk freely, participate fully, and live with dignity. “Ending stigma requires a united front,” he insists. “Only then can we create an environment where those affected can live with dignity and hope.” The seeds of change are already being planted, thanks to organizations like the Development Research and Advocacy Centre (DRAC). With support from Anesved Fundación, DRAC has drilled ten boreholes in Bongo and nearby communities, bringing clean and safe water to thousands. Water health committees now teach hygiene practices that are essential to fighting NTDs and breaking cycles of disease. But perhaps DRAC’s most transformative work lies in economic empowerment. Basket weaving and soap-making are not merely trades; they are lifelines. DRAC supplies materials, offers training, and connects artisans directly to buyers. “Buyers come to the community to purchase baskets, and we provide materials and training,” explains Executive Director Jonathan Adabre. For many, these initiatives restore not just income, but pride, purpose, and belonging. The story of Bongo’s leprosy patients and NTD survivors is, at its heart, a story of resilience. It is written in the determined footsteps of nurses on their rounds, the laughter of women weaving baskets, and the hope that flows with every borehole drilled. It is a story that calls for more than sympathy—it demands action, understanding, and a commitment to never again let these lives be forgotten. As the sun sets over Bongo, Tahiru Suleman’s voice continues to echo, a reminder that the true measure of a community is found in how it treats its most vulnerable. His fight is not just for awareness, but for acceptance; not just for support, but for solidarity. In breaking the chains of stigma, Bongo can become a place where everyone belongs, and where dignity is a right, not a reward. WATCH THE VIDEO DOCUMENTARY BELOW: Source: Apexnewsgh.com/Ngamegbulam Chidozie Stephen
DRAC’s Mission to Eradicate Neglected Tropical Diseases in Ghana’s Upper East
The quiet battle against Neglected Tropical Diseases (NTDs) is gathering new momentum. At the forefront of this fight is the Executive Development Research and Advocacy Centre (DRAC), an organization determined to bring health, hope, and dignity to some of the country’s most marginalized people. Apexnewsgh reports The story of DRAC’s mission unfolds in the documentary “Pains of the Forgotten: Leprosy, Stigma, and Resilience,” where Executive Director Jonathan Adabre shares his vision for a future free of the pain and stigma that have haunted families for generations. “We want to talk about the early manifestations of diseases like leprosy, meningitis, and yaws,” he explains. “If community members can recognize the signs, understand transmission, and know what treatment looks like, we can stop these illnesses before they destroy lives.” For decades, myths and misinformation have allowed diseases like leprosy to spread in silence. Many in the region still believe leprosy is hereditary, passed from mother to child—a belief that Adabre is determined to dispel. “Leprosy can take up to 20 years to show symptoms,” he clarifies. “A mother may unknowingly transmit it, and when her child develops symptoms much later, people assume it’s genetic. That’s the misconception we want to kill.” But the battle is not fought with education alone. DRAC’s strategy is deeply rooted in community collaboration. Chiefs, queen mothers, and local opinion leaders are enlisted as partners in the fight against stigma and discrimination. “We want affected persons to live dignified lives,” Adabre insists. “They should participate in community activities, share their views, and not be sidelined by fear.” Yet, changing minds is only part of the challenge. Inadequate sanitation and water access fuel the spread of NTDs. “Without water, people can’t wash, bathe, or keep their clothes clean. Transmission happens quietly,” Adabre notes. With support from the Anesvad Foundation, DRAC has drilled boreholes in several communities and established wetlands committees to manage these vital resources. The ripple effects are already being felt. A recent baseline survey conducted by DRAC revealed a sobering fact: 97% of respondents still practice open defecation, perpetuating health risks and undermining efforts to contain disease. To address this, DRAC is working closely with community health management committees and local leaders, pushing for behavioral change and better sanitation practices at every level. But health is only the foundation, DRAC recognizes that a future free of NTDs depends on economic empowerment as well. In many villages, basket weaving is part of the cultural heritage, but a lack of capital and market access keeps families in poverty. DRAC’s solution is to provide not just materials but direct connections to buyers, ensuring that the fruits of local labor reach wider markets. Training in soap and detergent making complements this initiative, promoting hygiene and providing an extra source of income. Crucially, DRAC’s work is shaped by the voices of those directly affected. “In this country, we have the habit of not listening to people before providing support,” Adabre observes. To change this, DRAC is helping form associations so that those living with NTDs, and their caregivers, can advocate for themselves. They share stories of stigma and exclusion, and highlight missed opportunities, such as the government’s LEAP program, which too often passes them by. Access to health care is another barrier DRAC is determined to break down. By partnering with the National Health Insurance Scheme (NHIS), the organization is bringing registration and renewal services directly to vulnerable populations, ensuring no one is left behind for lack of paperwork or travel money. The impact of DRAC’s approach is already apparent. Adabre recalls a striking moment from an awareness session: “An assembly member told us, ‘Are these signs really leprosy? I see them on my wife.’ When she was tested, it came back positive. That shows why early detection is critical.” For Mr. Adabre, the national goal is clear: “We want to eradicate skin NTDs in Ghana. It doesn’t take much, just consistent commitment and attention to the most vulnerable.” Through a blend of awareness-raising, improved water and sanitation, economic opportunity, and access to healthcare, DRAC is not just fighting disease; they are building resilience, breaking the cycle of stigma, and restoring hope to communities long forgotten. Their story is a call to action: that with compassion, partnership, and persistence, even the most neglected battles can be won. Source: Apexnewsgh.com/Ngamegbulam Chidozie Stephen
I don’t know why God gave me a disease that people don’t respect—Mr. Ayuumbeo leprosy patient, cries
Once upon a time, in the lively community of Bongo Soe, Mr. Adombire Ayuumbeo was the embodiment of diligence and pride. The sun’s first rays often found him by the dam near his house, tending to rows of tomatoes and vegetables. His farm was a patchwork of green, a source of sustenance for his family and a modest income from the surplus sold in the market. But farming was only a part of his industrious life; Mr. Ayuumbeo also spent hours cutting firewood and harvesting roofing grass, always ensuring his household’s needs were met. His hands, once strong and skilled, provided security, comfort, and hope to those who depended on him. This story, however, took a drastic turn. Leprosy crept silently into Mr. Ayuumbeo’s life, robbing him of the very tools of his trade, his fingers. The disease did not merely bring pain and disfigurement; it stripped him of his ability to work, leaving him “idle and helpless.” Once a man who never sat still, he now found himself confined to his home, watching the world move on without him. “When I remember the way I used to work and support my family, tears start pouring from my eyes,” Mr. Ayuumbeo confided in the documentary “Pains of the Forgotten: Leprosy, Stigma, and Resilience,” produced by Ngamegbulam Chidozie Stephen of ApexNewsGH. “Now I can’t farm, I can’t cut firewood, I can’t do anything. Sometimes I think I should die than to live.” For Mr. Ayuumbeo, the greatest agony is not only physical, but also the heavy shroud of stigma that leprosy brings. Once greeted with respect, he now feels abandoned and judged by the very people he once called neighbors and friends. “You don’t have anything, and your body too makes it hard to mingle with people. People stigmatize you. I don’t know why God gave me a disease that people don’t respect.” The sense of isolation is profound. The silence from others echoes louder than his disability, and the weight of judgment is heavier than any load he once carried from the fields. Despite these trials, Mr. Ayuumbeo tries to hold onto gratitude. “I thank God that the sores have healed and I can walk without difficulty. But I cannot do what I used to do.” His gratitude is laced with sorrow—a longing for lost strength, lost routine, and lost purpose. Each day, he wakes to face both the physical limitations of his body and the invisible barriers erected by society’s misunderstanding. His thoughts often return to his family. With a wife and children looking to him for support, the burden of helplessness is magnified. He worries about their future, how to keep them fed, clothed, and safe. “When I was active, I used to pay taxes. Now I cannot work, but I still belong to the government. I vote. I have my voter ID. The government of Ghana owes me and my family. If there’s any way they can help us sustain our lives, they should do it.” His appeal is not just for himself, but for every leprosy survivor who has been left behind, still a citizen, still deserving of dignity and support. Mr. Adombire’s story is woven into the larger tapestry of Bongo’s leprosy survivors—a tapestry colored by pain, but also by resilience and hope. Organizations like the Development Research and Advocacy Center (DRAC) are working to ensure that people like Mr. Ayuumbeo are not forgotten. DRAC’s efforts go beyond charity; they are about rebuilding lives. With the drilling of ten boreholes, clean water is now within reach for many who once struggled. Water health committees educate communities about hygiene, crucial in the fight against neglected tropical diseases. But perhaps most remarkable is DRAC’s commitment to economic empowerment. Training sessions in basket weaving and soap-making provide patients and caregivers with skills, materials, and, most importantly, a renewed sense of purpose. “Buyers come to the community to purchase baskets, and we provide materials and training,” says Jonathan Adabre, DRAC’s Executive Director. These initiatives are more than income; they are threads of dignity, restoring connections to the community and to self-worth. Across Bongo, the story of leprosy is changing. It is no longer solely a tale of suffering, but one of resilience written in the determined footsteps of a nurse on his rounds, in the laughter of women weaving baskets, and in the hope that arrives with every borehole drilled. Yet, Mr. Ayuumbeo’s plea still rings out, a call for compassion, inclusion, and meaningful action. His journey, and that of so many others, is a reminder that the scars of leprosy go beyond the physical. It is up to all, the community, government, and organizations, to ensure these lives are lifted from the silence of stigma into the light of dignity and support. Only then will the story of Bongo’s leprosy survivors be one not just of what was lost, but of what can still be regained. WATCH THE DOCUMENTARY VIDEO Source: Apexnewsgh.com/Ngamegbulam Chidozie Stephen
The Unseen Battles of Leprosy Survivors in Bongo
For ten long years, Matilda Nyaaba endured a mysterious torment. In her quiet village of Bongo Balungu, life was punctuated by fainting spells, nosebleeds, and unexplainable pain. Apexnewsgh reports Each episode left her weaker, and each visit to yet another health facility only compounded her confusion. What was this invisible enemy that drained her strength and hope, year after year? No one seemed to have an answer. Matilda’s ordeal was brought to light in the documentary “Pains of the Forgotten: Leprosy, Stigma, and Resilience,” produced by Ngamegbulam Chidozie Stephen of ApexNewsGH. Her story, like those of many leprosy sufferers, was one of searching in the dark. Even as her family stood by her, her neighbors whispered, eyed her with suspicion, and kept their distance. Some said she was cursed; others assumed she had HIV. To protect herself from the sting of their words, Matilda began to retreat indoors, leaving her home only for the most essential of chores. The isolation bit deeper than the disease itself, eroding her spirit and sense of belonging. It was only after a particularly harrowing episode, a collapse so severe she was rushed to the hospital, that a turning point arrived. There, a disease control officer finally recognized the signs of leprosy and placed Matilda on a monthly treatment regimen. For the first time, hope flickered in her life. The medicine brought relief, but not certainty. Supplies at the hospital ran out from time to time, and Matilda would wait anxiously for a call or a visit, never knowing when the next dose would arrive. Still, she persevered. Her wish was simple: that no one else should have to wander in confusion or suffer in silence as she had. Matilda’s journey reveals a truth often overlooked: the wounds of leprosy are as much emotional and social as they are physical. The pain of exclusion, the silence of misunderstood suffering, and the longing for dignity weigh heavily on those afflicted. Her resilience is a quiet call for compassion, understanding, and real action, so that no one else in her community will have to endure the same lonely road. Aniah’s Journey Through Leprosy’s Trials In the village of Bongo Soe, another story of quiet resilience unfolds. Aniah Lamisi was once a farmer whose days were filled with the rhythm of the land. She took pride in the sweep of her hoe, the bounty of her harvest, and the strength of her hands. Farming gave her purpose, connection, and identity. But leprosy crept into her life without warning, first as a tingling in her fingers, then as a relentless force that twisted and weakened her hands. Tasks that once came easily, cooking, fetching water, and gathering firewood, became daily struggles. The simple act of lifting a water container to her head was now a painful ordeal. Cooking over a fire brought blisters instead of warmth. With her hands disfigured, her independence slipped away, and Aniah found herself an observer in her own life, unable to work or contribute as she once did. The loss went deeper than the physical. Though her neighbors did not reject her outright, the shame of asking for help, of reaching out with altered hands for food, wounded her pride. She withdrew from communal life, carrying her pain in silence. Like Matilda, Aniah’s only hope was regular medication—but the health center’s supplies were unreliable. Some months, she received her treatment; other times, she waited in vain, watching her health and hope falter. Each missed dose was a reminder of how fragile her world had become. Yet Aniah’s spirit refused to break. In rare quiet moments, she counted her blessings: a body that still allowed her to dress herself, fleeting moments of calm, and the knowledge that others faced even greater struggles. She dreamed of something more, a chance to learn a trade, to regain purpose, to earn her own living. Vocational training, she thought, could be a bridge back to dignity and self-respect. While Matilda and Aniah’s stories are deeply personal, they are not unique. Across Bongo and its surrounding communities, many battle the same invisible foe, facing not just disease but the crushing weight of stigma, poverty, and uncertainty. But hope comes not only from within. Organizations like the Development Research and Advocacy Center (DRAC) are changing the landscape for leprosy patients. With ten boreholes drilled in affected areas, access to clean water is no longer a dream. Water health committees teach hygiene, helping prevent further spread of neglected tropical diseases. Most transformative are DRAC’s economic empowerment programs, training in basket weaving and soap-making, providing materials, and connecting patients with buyers. For women like Aniah and Matilda, these opportunities are more than a source of income; they are a path back to belonging and pride. The story of Bongo’s leprosy survivors is one of resilience, not just suffering. It is written in Matilda’s quiet hope, in Aniah’s determination, in every basket woven and every borehole drilled. It is a story that demands not pity, but recognition and commitment. For these women and countless others, the journey continues toward healing, dignity, and a future where no one must walk alone in the shadows. WATCH THE DOCUMENTARY VIDEO; Source: Apexnewsgh.com/Ngamegbulam Chidozie Stephen
A Journey of Compassion: The Unsung Heroes Battling Leprosy in Bongo
A battle is being fought, a struggle not only against disease, but against stigma, neglect, and despair. At the center of this fight is staff nurse David Asamani of the Bongo Soe Health Center, whose daily acts of compassion have transformed the lives of leprosy patients who have been forgotten by society. Apexnewsgh reports David Asamani is not just a nurse. To those he cares for, he is a lifeline, a confidant, and sometimes even family. While many health workers draw the boundaries of their duties at the clinic doors, Asamani’s responsibilities stretch far beyond. For him, the well-being of his patients does not end with the administration of medicine; it is a holistic mission that takes him across dusty roads and into the humble homes of those suffering from leprosy. The story of his devotion was brought to light during the documentary “Pains of the Forgotten: Leprosy, Stigma, and Resilience,” produced by Ngamegbulam Chidozie Stephen of ApexNewsGH. Asamani’s words echo the silent struggles of the people he serves: “Anytime I go to give them the medicine, I can see the suffering they are suffering,” he shares. The pain he describes is not just physical—but a deep emotional and social wound inflicted by poverty, isolation, and stigma. Many of Asamani’s patients live in the shadows, their disabilities making even the most basic tasks, cooking, cleaning, and earning a living, almost insurmountable. “Some of them will tell you they don’t even have food to eat while taking the medicine. Most of them don’t have anyone to help with household chores or economic activities; they just struggle on their own despite their disabilities.” One day, a new challenge arose. The district office called on leprosy patients to renew their health insurance and register for the government’s LEAP program. For most, this would mean a simple trip to town. But for these patients, left unsupported by family and shunned by their communities, it was an impossible journey. Asamani refused to let circumstances defeat them. “I had to use my motorbike to carry three of them to the district,” he recalls. The image is striking, a single nurse balancing duty and compassion, ferrying his patients toward a lifeline they could not reach alone. But compassion alone cannot fill empty medicine cupboards. Asamani’s dedication is tested time and again by the persistent shortages of vital drugs for leprosy and other neglected tropical diseases (NTDs). “Sometimes when patients need the medicine most, it is not available. By the time it comes, the harm has already been caused,” he laments. His plea is simple but urgent: “We will be grateful if the medicines could be available at all times. That will be very helpful.” Despite the government providing treatment for free, the reality on the ground is a different story. Attention is often focused elsewhere, and NTD patients find themselves at the bottom of the list. “Our concentration is on other diseases, neglecting these people. Meanwhile, these diseases cause a lot of economic challenges in our society. If we don’t take good care of them today, tomorrow you don’t know who might be affected,” Asamani warns, his voice carrying both frustration and hope. To Asamani, the fight against leprosy is not just medical, it is humanitarian. Each home visit, each ride on his motorbike, each moment spent listening to a patient’s worries, is a step toward restoring dignity and hope. His story is a powerful reminder that treating disease means more than dispensing drugs—it means confronting the poverty, stigma, and neglect that allow such illnesses to flourish. Yet, Asamani is not alone. The fight against leprosy in Bongo is bolstered by the work of the Development Research and Advocacy Center (DRAC), led by Executive Director Jonathan Adabre. DRAC’s approach is as holistic as Asamani’s devotion. With support from Anesved Fundación, DRAC raises awareness about the early signs of leprosy, elephantiasis, and yaws. “Many believe leprosy is genetic, but it takes up to 20 years to manifest. That misconception must end,” says Adabre. Their campaigns battle not only illness, but ignorance. DRAC’s impact is tangible. The organization has drilled ten boreholes across affected communities, ensuring access to clean and safe water. They have set up water health committees that teach hygiene practices, crucial in the fight against NTDs. But perhaps most transformative is their focus on economic empowerment. DRAC organizes training sessions in basket weaving and soap-making, providing materials and connecting patients and caregivers to markets. “Buyers come to the community to purchase baskets, and we provide materials and training,” Adabre notes. For many, these initiatives offer more than an income; they restore a sense of worth, dignity, and belonging. The story of Bongo’s leprosy patients is one of resilience, not just suffering. It is written in the determined footsteps of a nurse on his rounds, the laughter of women weaving baskets, and the hope that comes with every borehole drilled. It is a story that calls for more than sympathy; it demands action, understanding, and a commitment to never again let these lives be forgotten. WATCH THE VIDEO DOCUMENTARY: Source: Apexnewsgh.com/Ngamegbulam Chidozie Stephen
Stigmatization in Bongo is very high—District NTDs Focal Person
In the heart of Ghana’s Upper East Region, the Bongo District is fighting a quiet but devastating battle. Over the last six years, this rural district has recorded a deeply worrying rise in leprosy cases, with 57 new cases reported from 2019 to September 2025. For many, the word “leprosy” conjures up images from distant history books, but in Bongo, it is a daily reality, one made worse by stigma and isolation. This troubling revelation came from Mr. Kpankpari Wononuo Bismark, the District Neglected Tropical Diseases (NTDs) Focal Person, in the documentary “Pains of the Forgotten: Leprosy, Stigma, and Resilience” produced by Ngamegbulam Chidozie Stephen of ApexNewsGH. In a candid conversation, Mr. Bismark described the situation as “alarming,” drawing attention to the many layers of hardship leprosy patients endure beyond their diagnosis. “Stigmatization in Bongo is very high,” Mr. Bismark lamented. “Some patients are isolated, left in separate rooms, made to live alone. This worsens their mental health.” For many, the fear of being shunned by neighbors and loved ones is just as crippling as the disease itself. Some wait until their symptoms are too severe to hide, seeking help only when sores and deformities make life unbearable. “When we identify leprosy early, we can treat it within nine months,” Mr. Bismark explained. “But when patients report late with sores and deformities, the damage remains for life.” The consequences of this fear-driven delay are profound. Advanced leprosy often leaves patients with lifelong disabilities, making it impossible for them to farm or work. In a region where most people depend on their hands to earn a living, the economic toll can be just as devastating as the physical suffering. “Most of them cannot do meaningful work because of deformities,” Mr. Bismark said. “That is why interventions from NGOs that provide small capital for farming, weaving, or soap-making are so helpful. These initiatives help reduce idleness and restore dignity.” But the challenges don’t end with stigma and economics. Mr. Bismark also pointed to the struggles of accessing medicine, which must be requested from the regional health directorate and sometimes runs out. Still, he remains optimistic about the impact of treatment: “The good thing is that when we start the medicine, transmission to others is minimized, even though sometimes we run out of drugs briefly.” The changing climate also brings fresh hardships for leprosy patients. During the harsh dry season, cracked skin can lead to open sores that quickly become infected. Without easy access to clean water and proper hygiene, these sores can become septic, threatening not just health but life itself. “NTDs are neglected diseases, and sadly, the people suffering from them are also neglected,” Mr. Bismark noted. “Many patients live far from clean water sources, making hygiene very difficult.” Water, sanitation, and hygiene (WASH) remain critical challenges. In remote villages, fetching water involves long, painful journeys, a heavy burden for those already weakened by disease. This lack of WASH infrastructure leaves patients especially vulnerable to complications and further social exclusion. Despite these daunting obstacles, hope persists in the form of early detection and community support. “Leprosy is airborne, and elephantiasis is caused by mosquito bites. Everyone is at risk. That is why we keep telling the community: support patients, don’t stigmatize them, because you never know when you could also be affected,” Mr. Bismark urged. The fight against leprosy in Bongo is not waged by government alone. Non-governmental organizations like the Development Research and Advocacy Center (DRAC), led by Executive Director Jonathan Adabre, are helping to fill the gap. DRAC’s holistic approach tackles both the practical and social sides of the disease. “With support from Anesved Fundación, we raise awareness about early signs of diseases like leprosy, elephantiasis, and yaws,” Adabre explained. “Many believe leprosy is genetic, but it takes up to 20 years to manifest. That misconception must end.” DRAC’s projects are as varied as they are vital. The organization has drilled ten boreholes across affected communities, ensuring that more families have access to clean, safe water. They have also formed water health committees to educate locals on hygiene practices, crucial for managing NTDs. But perhaps their most transformative work lies in supporting economic empowerment. DRAC provides training and materials for basket weaving and soap-making, linking patients and caregivers to markets. “Buyers come to the community to purchase baskets, and we provide materials and training,” Adabre says. These initiatives offer more than income; they restore a sense of purpose and connection. The story of leprosy in Bongo is one of pain, but also of resilience and hope. It is a reminder that diseases like leprosy do not just attack the body, they disrupt families, livelihoods, and entire communities. Breaking the cycle requires more than medicine. It calls for compassion, early detection, and the kind of holistic support that brings patients out of the shadows and back into the embrace of their community. As Bongo continues its fight, the district’s journey stands as a testament to the power of partnership, awareness, and above all, human dignity. WATCH THE VIDEO DOCUMENTARY BELOW: Source: Apexnewsgh.com/Ngamegbulam Chidozie Stephen
Pains of the Forgotten: Leprosy, Stigma, and Resilience in Ghana–VIDEO ATTACHED
A documentary by Ngambebulam Chidozie-Stephen (ApexNewsGH) Editor in Chief Leprosy is one of humanity’s oldest diseases, yet in 2024, it remains a pressing global health crisis. According to the World Health Organization (WHO), 188 countries and territories reported a total of 172,717 new cases last year. The impact is not evenly distributed; women and girls comprised over 40% of new patients, and children accounted for more than 9,000 cases. Most troubling, over 9,100 new sufferers were diagnosed with the most severe form, grade 2 disability, a diagnosis that can mean permanent deformity and a lifetime of hardship. While leprosy’s global shadow is long, its most profound pain is felt in places like Ghana’s Upper East Region. Here, in the Bongo district, a community of just over 120,000 people, leprosy remains a silent threat. From 2019 to September 2025, 57 cases were officially reported, and the true number may be higher due to fear, stigma, and misunderstanding. Leprosy is just one of many Neglected Tropical Diseases (NTDs) that persist in Ghana. These diseases, fourteen of which are endemic in the country, disproportionately affect the poorest, deepening cycles of poverty and exclusion. Pain Behind Closed Doors: Matilda’s Story In the tight-knit community of Bongo Balungu, Matilda Nyaaba’s life is defined not only by the disease itself but by the isolation it breeds. For ten years, Matilda endured unexplained symptoms, fainting spells, nosebleeds, and growing weakness, a mystery to both her and the health professionals she visited. “Each episode left me weaker,” Matilda shares, remembering the confusion and fear that accompanied each new symptom. The only constant in her life became her monthly trips for medicine. Her family, she explains, has been a source of support, but the wider community’s reaction has been another story. She describes a self-imposed solitude, “I advised myself to stay indoors. They would use my condition against me.” Even basic errands, like fetching water from the borehole, are shadowed by the fear of being shunned. Whispers followed her: “Some described my illness as HIV, others as a curse. This has deeply affected my mental health; I don’t know what I’m thinking anymore.” Yet, Matilda’s resilience endures. She dreams of more than just survival: “If the government could help, maybe by providing vocational training, I could regain my dignity and hope for a brighter future.” From Provider to Dependent: Ania’s Struggle Before leprosy, Aniah Lamisi was at the center of her family’s livelihood in Bongo Soe. Farming was her pride and her purpose. But illness arrived quietly, a tingling in her fingers, followed by the slow, cruel twist of her hands. Aniah’s life shrank as the disease progressed. She could no longer wield a hoe or prepare meals over an open fire without pain. Even fetching water, a lifeline in the village, became a daily ordeal. She reflects on her new reality: “Some people have lost everything, even their mental faculties. I can still care for myself, dress well, and sometimes mingle with groups. That’s how I console myself. But if I can’t farm, how do I feed myself? I just sit and eat, if there’s food. Who will work for me?” Her appeal is simple but urgent. “If the government can provide us with a vocation or manual labor, we could earn a living. Now, I just wait and hope for food. Even cooking is painful, but who else will do it for me?” In Bongo Swing, Mr. Adombire Ayuumbeo once embodied industry and self-reliance. He farmed, cut firewood, and harvested thatch, supporting his family with pride. But when leprosy struck, it took his independence, disfigured his body, and left him idle. He describes the loss with raw honesty: “Everything I used to do to earn a living is gone. Now I am helpless. I sit alone. Nobody helps me. Sometimes I think it would be better to die than live like this. People stigmatize you. I don’t know why God gave me this disease that people don’t respect. When I remembered all these things happening to me, my tears began to fall.” He issues a plea not just for himself, but for others like him: “If the government can help sustain our lives, they should do it. I vote, I have a voting ID. If the government has anything to help, we would appreciate it.” The Sustainable Development Goals (SDGs), specifically Goal 3: Good Health and Well-being, address neglected tropical diseases (NTDs) like leprosy under Target 3.3. This target states: “By 2030, end the epidemics of AIDS, tuberculosis, malaria, and neglected tropical diseases, and combat hepatitis, waterborne diseases, and other communicable diseases.” This means that the global community, through the United Nations and its member states, has committed to eliminating NTDs, including leprosy, as public health problems by 2030. The aim is to reduce illness, disability, stigma, and death caused by these diseases through prevention, early detection, treatment, and improved access to health services, especially for vulnerable populations. In essence, the SDGs recognize that fighting NTDs is essential for achieving universal health coverage, reducing inequalities, and promoting the well-being of all people, particularly those living in poverty and marginalized communities. Ending NTDs like leprosy not only improves health outcomes but also supports broader development goals such as education, gender equality, and economic productivity. The rising trend of leprosy in Bongo is confirmed by Mr. Bismark Kpankpari Wononuo, the district’s Disease Control Officer, who doubles as the NTDs coordinator. He explained that the numbers increase every year. He credits increased detection to community volunteers but warns that the real challenge is stigma. According to him, “Many don’t come early for treatment due to discrimination. Early detection is key; if we treat early, within nine months, it can be cured. But when affected persons decide to report late, it causes deformities to remain for life.” He further sends a clear message to the community by letting them know that Leprosy is treatable and that early detection is crucial. “Everybody is at risk.” However, he acknowledged that there are
UER: 1190 cases of Yaws were suspected and treated between 2020 and 2024–GHS
The Upper East Regional Health Director, Dr. Braima Baba Abubakari, has highlighted a pressing public health concern in the region during the launch of the “Integrated Actions Towards Combating Skin NTDs in Ghana (NTDs Plus Project)” by Development Research and Advocacy Centre (DRAC). Apexnewsgh reports Leprosy and Yaws continue to affect many lives, with alarming statistics revealing the severity of the issue. A speech by the Regional Health Director indicates that between 2020 and 2024, the region detected 137 cases of Leprosy, with over 80% of patients reporting with advanced stages of disability. This indicates a significant delay in seeking medical attention, which can lead to long-term consequences. In the same period, approximately 1190 cases of Yaws were suspected and treated in the region. Dr. Abubakari expressed enthusiasm about the NTDs Plus Project, designed to address the challenges faced by individuals with Skin NTDs. The project leverages existing community structures to deliver health services, ensuring a comprehensive approach to tackling these diseases. The partnership between the health department and DRAC, supported by the Anesvad Foundation, is crucial to the project’s success. With the launch of the NTDs Plus Project, the Upper East region takes a significant step towards reducing the burden of Skin NTDs. By working together, stakeholders aim to improve health outcomes and enhance the quality of life for those affected by these diseases. The project’s success will depend on the collaborative efforts of all parties involved, and Dr. Abubakari expressed optimism about the positive impact it will have on the region. The Director of Programmes at DRAC, Mr. Aberinga Milton, announced that the NTDs Plus Project marks a significant milestone as the second phase of DRAC’s skin NTDs programming. The initial project, which targeted five districts in the Upper East Region – Binduri, Builsa South, Bongo, Nabdam, and Talensi – laid the groundwork for the new initiative. According to Mr. Aberinga, the NTDs Plus Project brings numerous improvements and benefits designed to support victims of skin NTDs and their communities. Mr. Aberinga highlighted the prevalence of specific health issues in certain areas of the region. Leprosy, he noted, is a significant concern in Bongo, while Yaws and other skin diseases are particularly prevalent in the Bolgatanga East area. These findings emphasize the need for targeted interventions to address these health challenges and improve the well-being of residents in these communities. With the NTDs Plus Project, DRAC is poised to build on its previous successes and make a meaningful impact in the lives of those affected by skin NTDs. The project’s improvements and benefits aim to provide comprehensive support to victims and their communities, ultimately contributing to a healthier and more resilient Upper East Region. The Bolgatanga Municipal Chief Executive’s representative, Presiding Member Mr. Stephen Akugre, officially launched the NTDs Plus Project on behalf of the MCE. At the launch, Mr. Akugre acknowledged the project’s potential impact and importance in Bolgatanga and the region as a whole. He expressed his support for the project, assuring DRAC that the MCE would work to ensure its success in the region. With a declaration, Mr. Akugre marked the official start of the NTDs Plus Project, paving the way for its implementation and anticipated positive outcomes. The Project launch saw the presence of Stakeholders from all the affected district and communities. Source: Apexnewsgh.com/ Ngamegbulam Chidozie Stephen
Empowering Persons with NTDs in Zorkor: KURADEC Provides Soap Making Training
In an effort to improve the lives of individuals affected by Neglected Tropical Diseases (NTDs) in Zorkor-Kadare, Bongo District, Upper East Region, Kunkua Renaissance Development Centre (KURADEC) has provided training in soap making. Apexnewsgh reports This economic and livelihood empowerment training aims to enhance the hygiene and development of persons with NTDs, enabling them to generate income and improve their overall well-being. Coordinator of KURADEC, Mr. Donatus Awine Adua, explained that the training is part of a larger initiative funded by ANESV Foundation through Development Research and Advocacy Center (DRAC). The goal is to equip affected individuals with skills to produce soap, which can be sold to generate income. Last year, KURADEC conducted LED intervention training for community volunteers and affected persons, identifying 65 beneficiaries, including men and women. NTDs, such as elephantiasis and hydrocele, expose affected individuals to vulnerabilities, including stigma, reduced mobility, and inability to access healthcare services. KURADEC’s training aims to address these challenges by promoting personal hygiene and economic empowerment. Mr. Adua appealed to other organizations and government agencies to prioritize support for persons with NTDs, particularly in rural areas. He emphasized the need for skills development and economic empowerment to improve their lives. KURADEC plans to provide additional support, including livestock, to enable beneficiaries to generate sustainable income. The organization encourages other NGOs and government agencies to join forces in empowering persons with NTDs, promoting a better quality of life for these vulnerable individuals. Freda Alowri, Midwife in charge of Zorko Health Centre, narrated how she witnessed firsthand the devastating impact of Neglected Tropical Diseases (NTDs) on individuals and communities. Despite the challenges, she remains committed to educating and empowering those affected to seek medical attention and improve their hygiene practices. The stigma surrounding NTDs, particularly leprosy, has led to many sufferers being ostracized and hidden away by their families. However, through home visits and community outreach, Freda and her team have managed to convince many to come forward and seek help. The introduction of soap making training has been a game-changer, providing economic empowerment and improving hygiene practices. Beneficiaries can now generate income by selling soap, and the community has come together to support those affected. Despite progress, challenges persist. Deep-seated mentalities and human behavior changes are difficult to overcome, and some individuals still hide their conditions due to shame or fear of association. Freda acknowledges the humanitarian efforts of organizations like Kunkua Renaissance Development Centre (KURADEC) and appeals for continued support to address the lingering challenges. She believes that together, they can make a significant impact and improve the lives of those affected by NTDs. The Zorko Health Centre’s dedication to combating NTDs has led to notable improvements in the community’s health and well-being. As Freda emphasizes, “We are not just treating conditions, we are restoring dignity and hope to those who need it most.” However, Janet Nsobila and Paul Awobgo beneficiaries of soap making activity could not hide their excitements. They extended their gratitude to Kunkua Renaissance Development Centre (KURADEC), Development Research and Advocacy Center (DRAC) and ANESV Foundation for such kind empowerment. Source: Apexnewsgh.com Thanks for reading from Apexnewsgh as a news publishing website from Ghana. We encourage you to freely share this story via social media platform and follow us on; Facebook on APEXNEWSGH-Tv or Please contact Apexnewsgh.com on email apexnewsgh@gmail.com for your credible news publications. Contact: 0248250270/0256336062