By Prof. Robert Baba Kuganab-Lem Introduction The government of Ghana have variously contemplated on how best to finance health care and all have tried to develop a system of financing that will reduce the financial limitations that cost of health care imposed on citizen’s access to health particularly the poor and vulnerable. Before independence access to health care was narrowed to expatriates and the few Ghanaians working with the public service. The government of Osygyefo Dr. Kwame Nkrumah established the Ghana Health Service. The object of the service was to open health care to all Ghanaians. The service included principles of health insurance and health care was free at the point of use. Prime Minister Abrefa Busia’s government in 1971 started charging for hospital services through the hospital fee act of 1971. The view of the government then was that the hospital fees will reduce unnecessary and health excessive use of health facilities and also raise some revenue for the facilities. This was not full cost recovery. Government still had to hugely subsidies health care. In the 1980s it became extremely difficult for government to fund health care. Government therefore introduced the Hospital Fees Regulation of 1985. This ushered in the principle of cost recovery. For the first time Ghanaians had to pay the cost of health care at the point of use. This fee regulation it was reported resulted in a drop in attendance at health facilities particularly in rural areas. The law was amended in 1990 and the law allowed health facilities to retain 100% of the revenue and also keep a revolving fund for drugs. It is this amendment that ushered in the term CASH and CARRY. In local parlance it connoted no money, no treatment. It was a very unpopular term. Several pieces of research point to a fact that some of the advantages of user fees were not materialised. It rather created problems of equity and for most of the population services were no longer affordable. Motivation for Health Insurance The Hospital Fees Regulation of 1985 (cost recovery) was largely resulting from structural adjustment programmes introduced by the World Bank and the IMF to correct balance of payment deficits. The act distorted the health seeking behaviour patterns of Ghanaians. The system placed a heavy financial burden on the poor and led to inequities in access to healthcare. But government had no option than to agree to cost recovery in an effort to stabilise the economy of the country, which had taken a nosedive. In other to mitigate the widening gap of access to health care, the government introduced an exemption policy in 1992. The essence of the policy was to exclude the poor and vulnerable from paying user fees. There were reports that that the exemption directive was hardly used. Service providers found the exemption policy cumbersome and laborious to implement. The inability of the exemption policy to work points to a known fact that all poor relief is given grudgingly and reluctantly by service providers. The regressive nature of the cash and carry policy, coupled with the lackadaisical implementation of the exemption policy resulted in diminishing access of the population to health care. This agitated government and non-governmental organisations considerably and thus the beginning of the exploration of a more equitable system for guaranteeing financial access to health care. The concept of health insurance in Ghana predates the establishment of the National Health Insurance Scheme (NHIS) and has its roots in community-based health insurance initiatives. Various community-based health insurance schemes (also known as mutual health insurance schemes) existed in Ghana, particularly in rural areas. These were small, localized efforts where community members pooled resources to pay for healthcare when needed. The Catholic Church played a very critical role in the establishment of health insurance in Ghana. The first and most successful scheme was the Nkoranza Community Health Insurance Scheme based at St Michael hospital in Nkoranza. The Catholics established through the support of GTZ at Damongo the Damongo Community Health insurance scheme. These schemes which started in the early 1990s became a model for community-based insurance schemes in other parts of the country. NDC and Health Insurance Agenda President Rawlings in 1995 in order to mitigate the regressive nature of the cash and carry system introduced the ideal of health insurance scheme by piloting a scheme at Dodowa. He then commissioned the Ministry of Health to undertake a feasibility study on community health insurance. The main thrust of the commissioned feasibility study was to provide policy-makers with relevant data on the demand for and feasibility of health insurance schemes. It was also to assist to formulate a health insurance policy that would suit the largely rural population within the Ghana socio-economic context. The government through the MoH received from a private consultancy group an explicit proposal in late 1995. This consultancy produced a comprehensive report on the feasibility for the establishment of a National Health Insurance in Ghana. The consultancy proposed strongly the establishment of a centralised national health insurance company for all contributors to the SSNIT and registered cocoa farmers. It also recommended pilot rural based community-financed schemes for the non-formal sector. The then government got SSNIT to establish a Subsidiary Company charged with the responsibility of piloting insurance schemes in the Eastern Region. In its 2000 manifesto the NDC stated that Health Insurance will be a major strategy for mobilising additional resources and for ensuring financial access to health care in time of need. They highlighted that the pilot work already carried out will form the basis for a mix of insurance schemes, both public and private, national and local to cater for salaried employees, the self-employed as well as both urban and rural communities. They further stated in the manifesto that one of the most effective ways of keeping the cost of health care to a minimum is through a Health Insurance Scheme and it is for this reason that the NDC Government conducted in-depth studies and pilot projects to facilitate
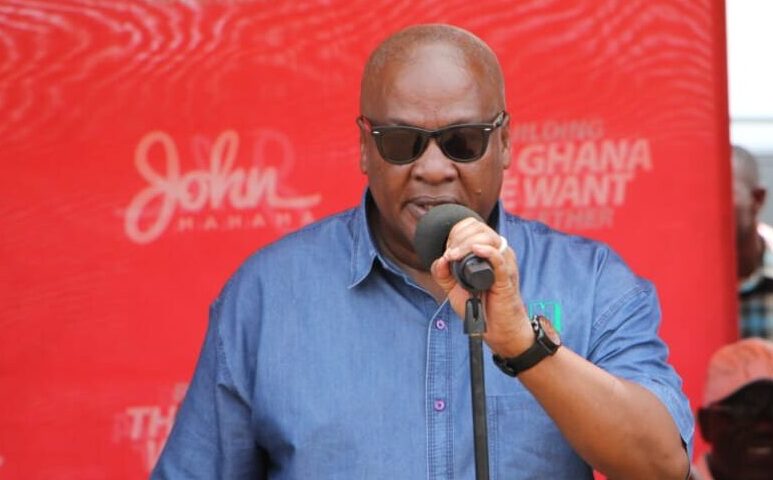
John Mahama mocks NHIS says, in Akufo-Addo Administration patients are denied paracetamol—John Dramani
Former President John Dramani Mahama has said, National Health Insurance card holders are denied common medicines at various hospitals across the country. The former President made the pronouncement in the Upper East Region during his two days official tour to meet with party delegates ahead of the upcoming Parliamentary primaries on May 13. Addressing delegates, the former President said: “As for National Health Insurance we don’t talk at all. It is simply not working and that is because the government is not refunding the claims of the hospital facilities after they have treated National Health Insurance holders. In our time, you could go with your National Health Insurance Card and you will be looked after, you go to the dispensary cough mixture, they will give you paracetamol, and they will give antibiotics. Today, if you go to the hospital after the look of things, you won’t get even paracetamol. You have to go and buy from the drug store, so NDC is coming to restore the National Health Insurance. We will make sure that the levy we collect goes to the purpose for which it will be used”. According to Mr. Mahama, what this government has done is that they have capped the National Health Insurance and so, when the money comes, they take some of it and for them to release it they won’t release it. For the last year or so they have not released any money to the National Health Insurance and so, we don’t what kind of government this is? He asked Source: Apexnewsgh.com/Ghana For publication please kindly contact us on 0256336062 or Email apexnewsgh@gmail.com